Are you gearing up for a career in Utilization Review Coordinator? Feeling nervous about the interview questions that might come your way? Don’t worry, you’re in the right place. In this blog post, we’ll dive deep into the most common interview questions for Utilization Review Coordinator and provide you with expert-backed answers. We’ll also explore the key responsibilities of this role so you can tailor your responses to showcase your perfect fit.
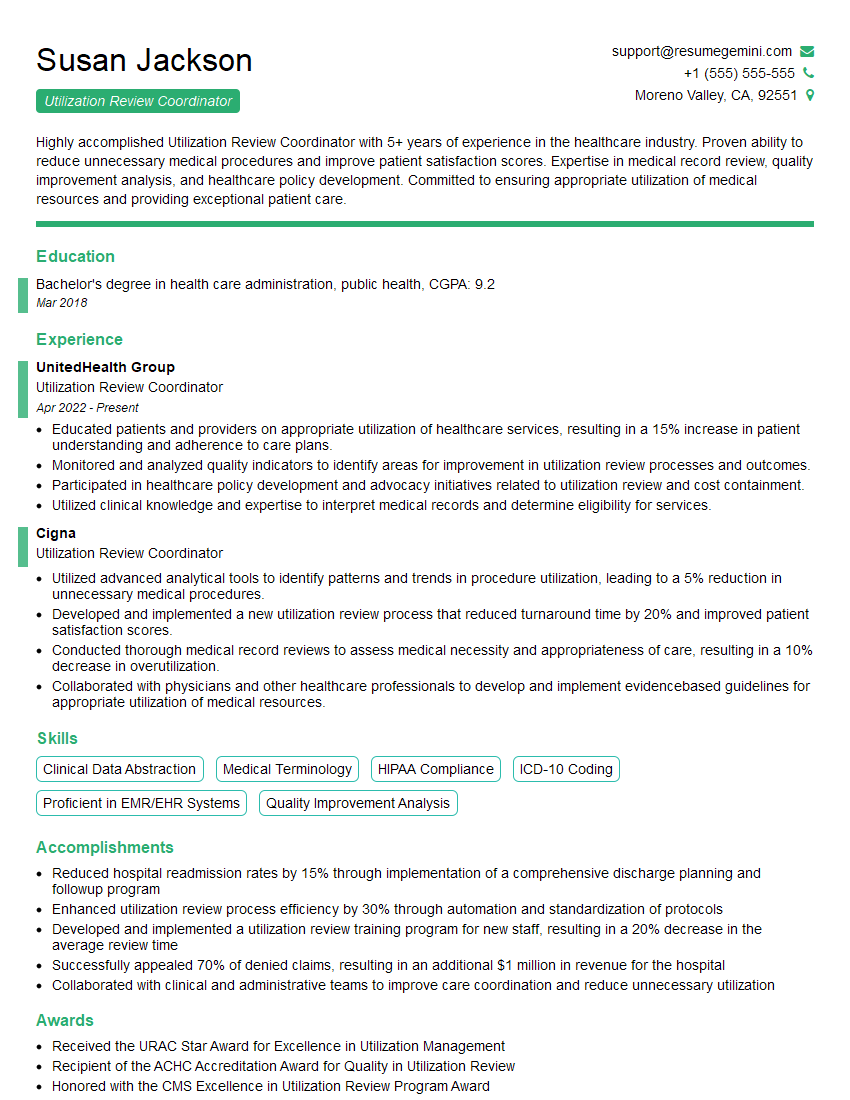
Acing the interview is crucial, but landing one requires a compelling resume that gets you noticed. Crafting a professional document that highlights your skills and experience is the first step toward interview success. ResumeGemini can help you build a standout resume that gets you called in for that dream job.
Essential Interview Questions For Utilization Review Coordinator
1. Can you describe the process of utilization review?
The utilization review process involves evaluating the appropriateness, necessity, and efficiency of healthcare services provided to patients. As a Utilization Review Coordinator, I would be responsible for assessing medical records, reviewing treatment plans, and conducting interviews with healthcare providers and patients to determine whether the services rendered are reasonable and in line with established medical guidelines. I would work closely with physicians, nurses, and other members of the healthcare team to ensure that patients receive the optimal level of care while minimizing unnecessary or inappropriate utilization of resources.
2. What are the key principles of utilization review?
Quality of Care
- Ensuring that patients receive appropriate, evidence-based care that meets their medical needs.
- Monitoring patient outcomes to identify and address any areas where care can be improved.
Cost-Effectiveness
- Evaluating whether the cost of healthcare services is commensurate with the benefits provided.
- Identifying ways to reduce unnecessary or wasteful spending while maintaining a high standard of care.
Patient Satisfaction
- Involving patients in the utilization review process to ensure that their perspectives and concerns are considered.
- Providing clear and timely communication to patients regarding utilization review decisions.
3. What are the common challenges faced in utilization review?
Some common challenges encountered in utilization review include:
- Balancing the need for cost-effective care with the provision of high-quality services that meet patient needs.
- Interpreting complex medical information and guidelines to make appropriate utilization decisions.
- Addressing potential conflicts of interest between healthcare providers, insurers, and patients.
- Keeping up-to-date with evolving medical practices and technologies.
- Managing a large volume of cases while ensuring timely and accurate review
4. How do you stay up-to-date with the latest developments in healthcare and utilization review best practices?
To stay current with the latest developments in healthcare and utilization review best practices, I engage in continuous professional development activities, such as:
- Attending conferences, workshops, and webinars on utilization review.
- Reading peer-reviewed journals and research articles.
- Participating in online discussion forums and networking with other utilization review professionals.
- Seeking out opportunities for mentorship and guidance from experienced colleagues.
5. What is your understanding of the role of technology in utilization review?
Technology plays a crucial role in modern utilization review processes. I am proficient in utilizing various software applications and tools to enhance my efficiency and effectiveness. These tools can assist with:
- Automating data collection and analysis, reducing manual workload.
- Facilitating collaboration among team members and healthcare providers.
- Providing access to real-time data and analytics for decision-making.
- Improving the accuracy and consistency of utilization review determinations.
6. How do you handle situations where you have to deny a patient’s request for a particular treatment or service?
When faced with the need to deny a patient’s request for a particular treatment or service, I approach the situation with empathy and professionalism. I take the following steps:
- Clearly explain the reason for the denial, referring to specific medical guidelines or evidence-based criteria.
- Discuss alternative treatment options or services that may be more appropriate.
- Listen attentively to the patient’s concerns and provide a space for them to express their feelings.
- Offer resources or support services that can assist the patient in obtaining the care they need.
7. Can you describe a time when you identified a potential case of fraud or abuse in utilization review?
In a previous role, I encountered a case where a provider was submitting excessive claims for services that were not medically necessary. I noticed a pattern of unusually high utilization rates and discrepancies in the documentation. Through thorough investigation, I gathered evidence and collaborated with the fraud investigation team to report the provider’s actions.
8. How do you ensure fairness and objectivity in your utilization review decisions?
To ensure fairness and objectivity in my utilization review decisions, I adhere to the following principles:
- Relying on evidence-based guidelines and medical criteria.
- Evaluating each case individually, considering the patient’s unique circumstances.
- Consulting with physicians and other healthcare professionals when necessary.
- Documenting all decisions clearly and providing rationale for my findings.
- Undergoing regular training and continuing education to enhance my knowledge and skills.
9. Can you explain the concept of medical necessity in utilization review?
Medical necessity refers to healthcare services or treatments that are essential for the diagnosis, treatment, or prevention of illness, injury, or disability. In utilization review, I assess whether services meet the criteria of medical necessity by considering:
- The patient’s medical condition and symptoms.
- The appropriateness of the treatment plan.
- The availability of alternative, less costly treatments.
- The potential risks and benefits of the treatment.
10. How do you handle disagreements with healthcare providers regarding utilization review decisions?
When faced with disagreements with healthcare providers regarding utilization review decisions, I approach the situation professionally and respectfully. I take the following steps:
- Schedule a meeting with the provider to discuss the rationale behind the decision.
- Present the evidence and guidelines supporting my findings.
- Listen attentively to the provider’s perspective and concerns.
- Collaborate to explore alternative solutions or treatment options that meet both medical necessity and cost-effectiveness.
- Document the discussion and any agreed-upon modifications to the decision.
Interviewers often ask about specific skills and experiences. With ResumeGemini‘s customizable templates, you can tailor your resume to showcase the skills most relevant to the position, making a powerful first impression. Also check out Resume Template specially tailored for Utilization Review Coordinator.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Great Savings With New Year Deals and Discounts! In 2025, boost your job search and build your dream resume with ResumeGemini’s ATS optimized templates.
Researching the company and tailoring your answers is essential. Once you have a clear understanding of the Utilization Review Coordinator‘s requirements, you can use ResumeGemini to adjust your resume to perfectly match the job description.
Key Job Responsibilities
A Utilization Review Coordinator is responsible for various tasks related to managing and coordinating the utilization review process. This role plays a critical part in ensuring that medical services and treatments are appropriate, necessary, and cost-effective.
1. Medical Record Review
Reviews medical records, including physician orders, progress notes, and test results, to assess the medical necessity and appropriateness of services, procedures, and treatments.
2. Case Management
Coordinates with providers, nurses, and other healthcare professionals to gather additional information, clarify treatment plans, and monitor patient outcomes.
3. Data Analysis
Analyzes utilization data to identify patterns, trends, and areas for improvement in healthcare resource utilization.
4. Quality Assurance
Participates in quality assurance activities, such as peer review and performance improvement initiatives, to ensure the accuracy and consistency of utilization review decisions.
5. Regulatory Compliance
Maintains compliance with regulatory guidelines and standards governing utilization review, including HIPAA and Medicare guidelines.
Interview Preparation Tips
To prepare for an interview for a Utilization Review Coordinator position, consider the following tips:
1. Research the Company and Position
Familiarize yourself with the healthcare organization and the specific responsibilities of the Utilization Review Coordinator role. This will help you tailor your answers to demonstrate your understanding of the company’s needs and goals.
2. Highlight Your Qualifications
Emphasize your experience in medical record review, case management, and data analysis. Quantify your accomplishments whenever possible. For example, instead of saying “I analyzed utilization data,” say “I identified a 10% reduction in unnecessary hospital readmissions through data analysis.”
3. Demonstrate Your Communication Skills
Utilization Review Coordinators need excellent communication skills to interact with healthcare professionals, patients, and insurance companies. Highlight your ability to clearly articulate complex medical information and communicate effectively in both written and verbal formats.
4. Show Your Commitment to Quality
Emphasize your commitment to providing high-quality healthcare and your understanding of the importance of utilization review in ensuring appropriate and cost-effective care. Discuss your involvement in any quality improvement initiatives or your previous experience in maintaining regulatory compliance.
5. Be Prepared for Behavioral Questions
In addition to technical questions about utilization review, you may also be asked behavioral questions such as: “Tell me about a time when you had to resolve a difficult situation with a provider.” Prepare for these questions by practicing your answers and providing specific examples of your skills and experiences.
Next Step:
Now that you’re armed with a solid understanding of what it takes to succeed as a Utilization Review Coordinator, it’s time to turn that knowledge into action. Take a moment to revisit your resume, ensuring it highlights your relevant skills and experiences. Tailor it to reflect the insights you’ve gained from this blog and make it shine with your unique qualifications. Don’t wait for opportunities to come to you—start applying for Utilization Review Coordinator positions today and take the first step towards your next career milestone. Your dream job is within reach, and with a polished resume and targeted applications, you’ll be well on your way to achieving your career goals! Build your resume now with ResumeGemini.