Are you gearing up for a career in Clinical Documentation Improvement Specialist (CDIS)? Feeling nervous about the interview questions that might come your way? Don’t worry, you’re in the right place. In this blog post, we’ll dive deep into the most common interview questions for Clinical Documentation Improvement Specialist (CDIS) and provide you with expert-backed answers. We’ll also explore the key responsibilities of this role so you can tailor your responses to showcase your perfect fit.
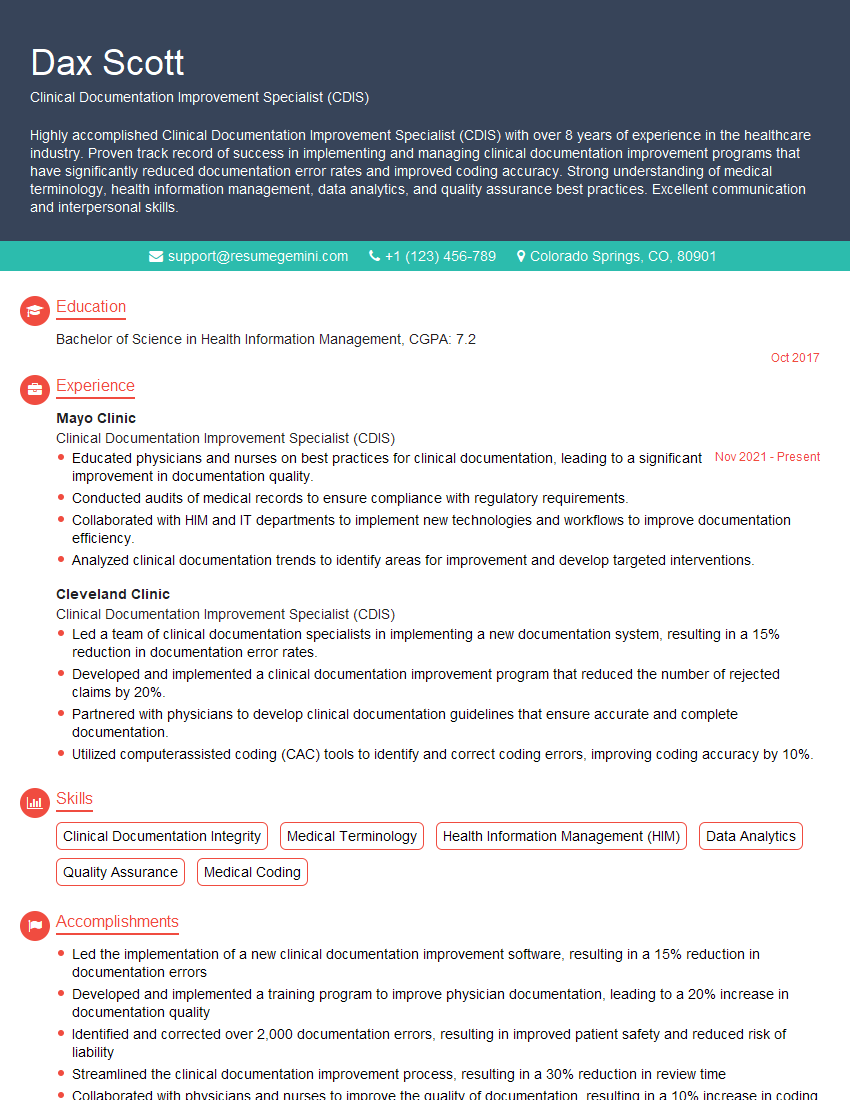
Acing the interview is crucial, but landing one requires a compelling resume that gets you noticed. Crafting a professional document that highlights your skills and experience is the first step toward interview success. ResumeGemini can help you build a standout resume that gets you called in for that dream job.
Essential Interview Questions For Clinical Documentation Improvement Specialist (CDIS)
1. Define clinical documentation improvement (CDI) and elaborate its main goals and objectives.
- CDI is a process of improving the quality of clinical documentation by ensuring that the medical records are complete, accurate, and compliant with regulatory requirements.
- Main goals and objectives of CDI include:
- Improving patient care by ensuring that the medical records contain all the necessary information to support clinical decision-making.
- Reducing the risk of medical errors by identifying and correcting inaccurate or incomplete documentation.
- Improving the quality of data used for research and quality improvement initiatives.
- Ensuring compliance with regulatory requirements, such as the Health Insurance Portability and Accountability Act (HIPAA) and the Joint Commission.
2. Explain the principles of CDI and discuss how they are applied in practice.
Key principles of CDI:
- Completeness: Ensuring that the medical record contains all the necessary information to support clinical decision-making.
- Accuracy: Ensuring that the information in the medical record is correct and up-to-date.
- Timeliness: Ensuring that the information in the medical record is available when it is needed.
- Compliance: Ensuring that the medical record meets all regulatory requirements.
Application of CDI principles in practice:
- CDI specialists review medical records to identify any areas where the documentation is incomplete, inaccurate, or non-compliant.
- The CDI specialist then works with the physician to obtain the necessary information to complete the documentation.
- The CDI specialist may also provide education to physicians and other healthcare providers on the importance of accurate and complete documentation.
3. Describe the different types of documentation that a CDIS typically reviews.
- Patient medical records, including history and physical exams, progress notes, discharge summaries, and operative reports.
- Quality assurance reports, such as chart audits and performance improvement reports.
- Coding reports, such as DRG validation reports and ICD-10-CM/PCS reports.
- Regulatory reports, such as HIPAA compliance reports and Joint Commission surveys.
4. Explain the role of a CDIS in coding accuracy and how they contribute to the overall quality of the hospital’s data.
- CDISs play a vital role in coding accuracy by ensuring that the medical records contain all the necessary information to support the assigned codes.
- They also work with coders to ensure that the codes are assigned correctly based on the documentation.
- By improving the quality of the documentation, CDISs can help to ensure that the hospital’s data is accurate and complete, which is essential for quality improvement initiatives and research.
5. Discuss the importance of interdisciplinary collaboration in CDI and provide examples of how it can improve patient care.
- Interdisciplinary collaboration is essential for CDI because it allows CDISs to access the expertise of other healthcare professionals, such as physicians, nurses, and coders.
- By working together, these professionals can ensure that the medical records are complete, accurate, and compliant with regulatory requirements.
- For example, a CDIS may work with a physician to obtain a clarification on a diagnosis, or they may work with a coder to ensure that the correct code is assigned to a procedure.
- Interdisciplinary collaboration can also improve patient care by reducing the risk of medical errors and improving the quality of data used for research and quality improvement initiatives.
6. Describe the ethical considerations and legal responsibilities associated with the role of a CDIS.
Ethical considerations:
- CDISs must maintain confidentiality of patient information.
- They must also be objective and unbiased in their review of medical records.
- CDISs should avoid conflicts of interest, such as working with a physician who is a family member or friend.
Legal responsibilities:
- CDISs must comply with all applicable laws and regulations, such as HIPAA and the Joint Commission.
- They may be required to testify in court or provide depositions if they are involved in a legal case.
7. How do you stay up-to-date with the latest changes in medical terminology, coding guidelines, and regulatory requirements?
- Attending conferences and workshops
- Reading professional journals and books
- Taking online courses
- Participating in webinars
- Networking with other CDISs and healthcare professionals
8. What are your strengths and weaknesses as a CDIS?
Strengths:
- Excellent attention to detail
- Strong understanding of medical terminology and coding guidelines
- Proven ability to work independently and as part of a team
- Excellent communication and interpersonal skills
Weaknesses:
- Limited experience with a specific EHR system
- Not yet certified as a CDIS
9. Why are you interested in this position?
- I am passionate about improving the quality of patient care, and I believe that CDI is a vital part of that process.
- I am confident that I have the skills and experience to be a successful CDIS, and I am eager to learn more about this position.
- I am confident that I can make a significant contribution to your team and help to improve the quality of care at your hospital.
10. What are your salary expectations?
- My salary expectations are in line with the market rate for CDISs in this area.
- I am also willing to negotiate based on the benefits package and the overall compensation package.
Interviewers often ask about specific skills and experiences. With ResumeGemini‘s customizable templates, you can tailor your resume to showcase the skills most relevant to the position, making a powerful first impression. Also check out Resume Template specially tailored for Clinical Documentation Improvement Specialist (CDIS).
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Great Savings With New Year Deals and Discounts! In 2025, boost your job search and build your dream resume with ResumeGemini’s ATS optimized templates.
Researching the company and tailoring your answers is essential. Once you have a clear understanding of the Clinical Documentation Improvement Specialist (CDIS)‘s requirements, you can use ResumeGemini to adjust your resume to perfectly match the job description.
Key Job Responsibilities
Clinical Documentation Improvement Specialists (CDIS), also known as clinical documentation integrity specialists, are responsible for reviewing medical records to ensure that they are accurate, complete, and compliant with regulatory standards. They work closely with healthcare providers to improve the quality of documentation, which can lead to better patient care and reduced costs.
1. Review and Analyze Medical Records
CDISs review medical records to identify any errors or omissions. They also check to make sure that the documentation is complete and meets all regulatory requirements.
- Identify errors or omissions in medical records
- Ensure that documentation is complete and meets all regulatory requirements
2. Query Healthcare Providers for Missing or Incorrect Information
If a CDIS finds any errors or omissions in the medical record, they will query the healthcare provider for the correct information. They will also work with the provider to clarify any ambiguous or incomplete information.
- Query healthcare providers for missing or incorrect information
- Clarify any ambiguous or incomplete information
3. Educate Healthcare Providers on Documentation Best Practices
CDISs can help to improve the quality of documentation by educating healthcare providers on best practices. They can provide training on how to document accurately and completely, and they can also answer any questions that providers may have.
- Provide training on how to document accurately and completely
- Answer any questions that providers may have
4. Implement and Maintain Documentation Improvement Programs
CDISs can help to implement and maintain documentation improvement programs. These programs can help to improve the quality of documentation throughout the organization, and they can also help to reduce the risk of errors or omissions.
- Implement and maintain documentation improvement programs
- Reduce the risk of errors or omissions
Interview Tips
A successful interview requires preparation and practice. Here are some tips to help you ace your interview for a Clinical Documentation Improvement Specialist position:
1. Research the Company and the Position
Before you go into your interview, take some time to research the company and the position. This will help you to understand the company culture and the specific requirements of the role.
- Visit the company website
- Read the job description carefully
- Look for news articles or press releases about the company
2. Practice Your Answers to Common Interview Questions
There are a few common interview questions that you are likely to be asked in an interview for a Clinical Documentation Improvement Specialist position. These questions include:
- Why are you interested in this position?
- What is your experience with clinical documentation improvement?
- How do you stay up-to-date on the latest changes in healthcare regulations?
- What are your strengths and weaknesses as a Clinical Documentation Improvement Specialist?
3. Prepare Questions to Ask the Interviewer
At the end of the interview, the interviewer will likely ask if you have any questions. This is your chance to learn more about the position and the company. Some good questions to ask include:
- What are the biggest challenges facing Clinical Documentation Improvement Specialists today?
- What are the opportunities for professional development within the company?
- What is the company culture like?
4. Dress Professionally and Arrive on Time
First impressions matter, so it is important to dress professionally and arrive on time for your interview. This shows the interviewer that you are respectful of their time and that you are serious about the position.
- Dress in business attire
- Arrive on time for your interview
- Be polite and respectful to the interviewer
Next Step:
Now that you’re armed with a solid understanding of what it takes to succeed as a Clinical Documentation Improvement Specialist (CDIS), it’s time to turn that knowledge into action. Take a moment to revisit your resume, ensuring it highlights your relevant skills and experiences. Tailor it to reflect the insights you’ve gained from this blog and make it shine with your unique qualifications. Don’t wait for opportunities to come to you—start applying for Clinical Documentation Improvement Specialist (CDIS) positions today and take the first step towards your next career milestone. Your dream job is within reach, and with a polished resume and targeted applications, you’ll be well on your way to achieving your career goals! Build your resume now with ResumeGemini.