Are you gearing up for a career shift or aiming to ace your next interview? Look no further! We’ve curated a comprehensive guide to help you crack the interview for the coveted Credentialing Specialist position. From understanding the key responsibilities to mastering the most commonly asked questions, this blog has you covered. So, buckle up and let’s embark on this journey together.
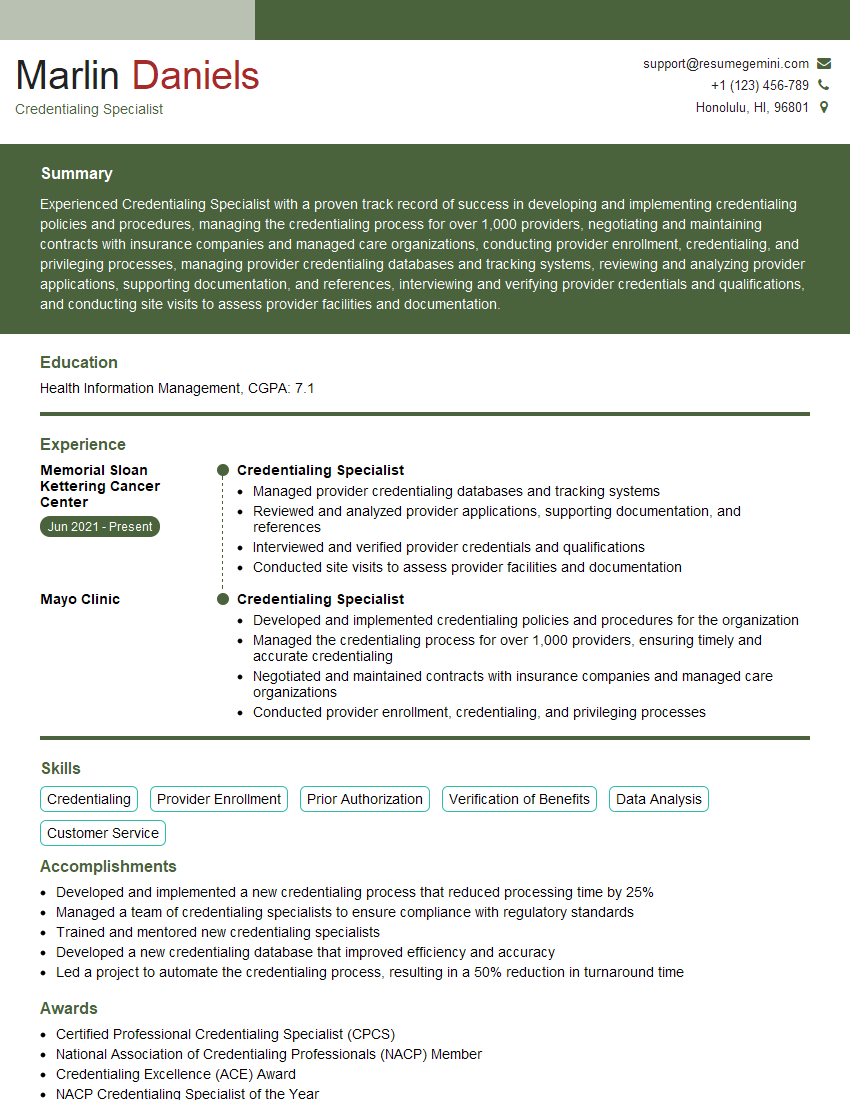
Acing the interview is crucial, but landing one requires a compelling resume that gets you noticed. Crafting a professional document that highlights your skills and experience is the first step toward interview success. ResumeGemini can help you build a standout resume that gets you called in for that dream job.
Essential Interview Questions For Credentialing Specialist
1. What are the key steps involved in the credential verification process?
- Gather required documentation (e.g., diplomas, licenses, certifications)
- Verify the authenticity and validity of the documents
- Contact source institutions to confirm issuing status and details
- Assess and interpret credential information for completeness and accuracy
- Generate a comprehensive credentialing report or summary
2. How do you ensure the confidentiality and security of protected health information (PHI) during the credential verification process?
Compliance with HIPAA
- Adhere to HIPAA privacy and security regulations
- Use secure methods for data transmission and storage
Internal Policies and Procedures
- Implement and enforce strict policies and procedures
- Limit access to PHI to authorized personnel only
- Regularly audit and monitor systems to prevent unauthorized access or breaches
3. Describe the role of the National Provider Identifier (NPI) in credential verification.
- Unique identifier assigned to individual healthcare providers
- Used for identification in various healthcare transactions
- Helps verify provider credentials and prevent fraud and abuse
4. How do you handle discrepancies or inconsistencies found during credential verification?
- Contact source institutions for clarification or additional documentation
- Request a signed affidavit or explanation from the provider
- Review state and national databases for any disciplinary actions or complaints
- Document all findings and communications for transparency and accountability
5. What technologies or tools do you use to streamline and enhance the credentialing process?
- Credentialing software or platforms for automation and data management
- Online verification tools for real-time access to provider information
- Digital signature and document management systems for secure and efficient workflows
- Data analytics tools for identifying trends and improving processes
6. How do you stay updated on changes in credentialing regulations and requirements?
- Attend industry conferences and webinars
- Subscribe to relevant publications and newsletters
- Participate in professional organizations and networking groups
- Utilize online resources and databases for the latest information
7. How do you prioritize and manage a large volume of credentialing applications?
- Establish clear triage protocols based on urgency and importance
- Use technology to automate tasks and streamline workflows
- Delegate responsibilities and collaborate with colleagues
- Implement quality control measures to ensure accuracy and efficiency
8. What are the common challenges and roadblocks you encounter in credentialing?
- Incomplete or inconsistent applications
- Delays in responses from source institutions
- Discrepancies in provider information
- Changes in credentialing regulations and requirements
- Managing a high volume of applications
9. How do you ensure the accuracy and completeness of the credentialing report?
- Thorough review of all gathered documentation
- Verification of information through multiple sources
- Attention to detail and careful analysis of data
- Double-checking and cross-referencing findings
- Proofreading and editing the final report
10. How do you collaborate with providers and other stakeholders during the credentialing process?
- Communicate regularly with providers to gather necessary information and address any queries
- Work closely with HR and other departments to ensure alignment with organizational policies
- Maintain open lines of communication with external stakeholders (e.g., licensing boards)
- Build relationships and foster trust through professionalism and responsiveness
Interviewers often ask about specific skills and experiences. With ResumeGemini‘s customizable templates, you can tailor your resume to showcase the skills most relevant to the position, making a powerful first impression. Also check out Resume Template specially tailored for Credentialing Specialist.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Great Savings With New Year Deals and Discounts! In 2025, boost your job search and build your dream resume with ResumeGemini’s ATS optimized templates.
Researching the company and tailoring your answers is essential. Once you have a clear understanding of the Credentialing Specialist‘s requirements, you can use ResumeGemini to adjust your resume to perfectly match the job description.
Key Job Responsibilities
Credentialing Specialists are responsible for managing the credentialing process for healthcare providers to ensure they meet the requirements of insurance companies and government agencies. Their key job responsibilities include:
1. Credentialing and Re-credentialing
Gathering and verifying provider credentials, including licenses, certifications, and malpractice insurance.
- Processing and submitting credentialing applications to insurance companies and government agencies.
- Tracking the status of credentialing applications and following up with insurance companies and government agencies as needed.
2. Provider Enrollment
Enrolling providers with insurance companies and government agencies to allow them to bill for services.
- Verifying provider information and ensuring it matches the information on credentialing applications.
- Submitting provider enrollment applications to insurance companies and government agencies.
- Tracking the status of provider enrollment applications and following up with insurance companies and government agencies as needed.
3. Data Management
Maintaining accurate and up-to-date provider data in the organization’s credentialing system.
- Updating provider information as needed.
- Generating reports on credentialing and provider enrollment status.
- Providing data to other departments within the organization as needed.
4. Compliance
Ensuring that the organization is in compliance with all applicable credentialing and provider enrollment laws and regulations.
- Staying up-to-date on changes to credentialing and provider enrollment laws and regulations.
- Developing and implementing policies and procedures to ensure compliance.
- Conducting audits to ensure compliance.
Interview Tips
To ace the interview for a Credentialing Specialist position, there are several tips and preparation strategies you can follow:
1. Research the Organization and Position
Thoroughly review the job description and identify the key responsibilities and qualifications required for the position. Visit the company website to learn about its mission, values, and culture. This knowledge will help you tailor your answers to the interviewer’s questions and demonstrate your understanding of the role.
- Prepare specific examples from your previous experience that highlight your skills and abilities in each of the key job responsibilities.
- Use the STAR method (Situation, Task, Action, Result) to structure your answers and provide clear and concise explanations of your accomplishments.
2. Practice Common Interview Questions
Anticipate the common interview questions you may be asked and prepare your responses in advance. Here are some examples:
- Tell me about your experience in credentialing and provider enrollment.
- How do you stay up-to-date on changes to credentialing and provider enrollment laws and regulations?
- How do you handle difficult situations with insurance companies or government agencies?
3. Be Prepared to Talk About Your Skills and Abilities
Highlight your skills and abilities relevant to the position, including:
- Strong communication and interpersonal skills.
- Excellent organizational and time management skills.
- Attention to detail and accuracy.
- Proficiency in using credentialing software and systems.
- Understanding of healthcare regulations and compliance.
4. Be Enthusiastic and Professional
Throughout the interview, maintain a positive and enthusiastic attitude. Dress professionally and arrive on time for your interview. Be polite and respectful to the interviewer, and thank them for their time.
- Show your passion for the healthcare industry and your commitment to providing excellent patient care.
- Be prepared to discuss your career goals and how this position aligns with them.
Next Step:
Now that you’re armed with interview-winning answers and a deeper understanding of the Credentialing Specialist role, it’s time to take action! Does your resume accurately reflect your skills and experience for this position? If not, head over to ResumeGemini. Here, you’ll find all the tools and tips to craft a resume that gets noticed. Don’t let a weak resume hold you back from landing your dream job. Polish your resume, hit the “Build Your Resume” button, and watch your career take off! Remember, preparation is key, and ResumeGemini is your partner in interview success.