Are you gearing up for a career shift or aiming to ace your next interview? Look no further! We’ve curated a comprehensive guide to help you crack the interview for the coveted Diabetes Education Coordinator position. From understanding the key responsibilities to mastering the most commonly asked questions, this blog has you covered. So, buckle up and let’s embark on this journey together.
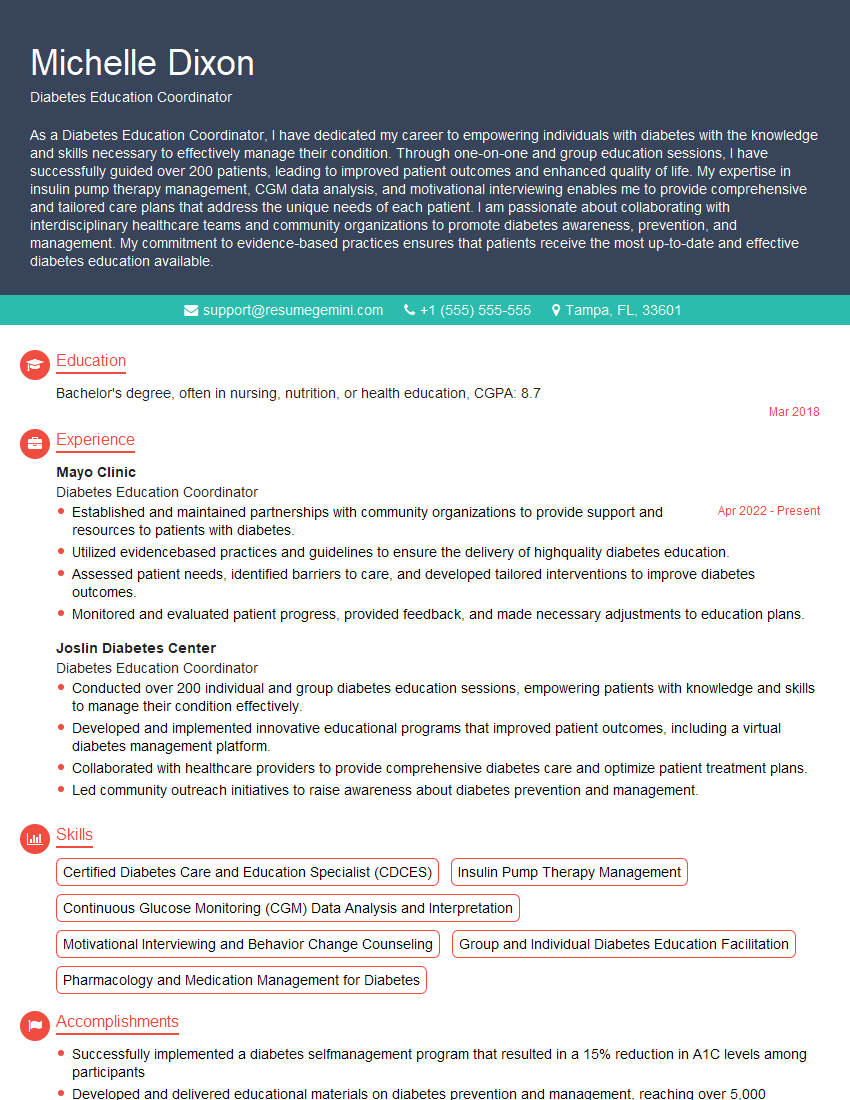
Acing the interview is crucial, but landing one requires a compelling resume that gets you noticed. Crafting a professional document that highlights your skills and experience is the first step toward interview success. ResumeGemini can help you build a standout resume that gets you called in for that dream job.
Essential Interview Questions For Diabetes Education Coordinator
1. What is your understanding of the role of a Diabetes Education Coordinator?
The primary role of a Diabetes Education Coordinator is to provide comprehensive education and support to individuals with diabetes, their families, and the community. As a Diabetes Education Coordinator, my responsibilities include:
- Providing education on diabetes management, including nutrition, medication, exercise, and lifestyle modifications
- Assessing patients’ needs and developing individualized care plans
- Teaching self-management skills to patients and their families
- Supporting patients in making informed decisions about their diabetes care
- Collaborating with other healthcare professionals to provide comprehensive care
2. How would you approach educating a newly diagnosed patient about diabetes management?
Patient education
- Start by establishing a rapport and assessing the patient’s knowledge and understanding of diabetes.
- Provide clear and concise information about what diabetes is, its causes, and its management.
- Use visual aids, handouts, and interactive tools to make the information accessible and engaging.
- Tailor the information to the patient’s individual needs, learning style, and cultural background.
- Encourage questions and provide opportunities for practice.
Support and resources
- Provide emotional support and encouragement to the patient.
- Help the patient identify and connect with support groups and resources.
- Refer the patient to other healthcare professionals, such as a dietitian or psychologist, as needed.
- Follow up with the patient regularly to assess their progress and provide ongoing support.
3. What are the key elements of a successful diabetes management program?
- Patient-centered approach: Tailoring the program to the individual needs and preferences of each patient.
- Comprehensive education: Covering all aspects of diabetes management, including nutrition, medication, exercise, lifestyle modifications, and emotional support.
- Skill training: Teaching patients essential self-management skills, such as blood glucose monitoring, insulin administration, and meal planning.
- Emotional support: Providing a supportive and encouraging environment where patients feel comfortable asking questions, sharing experiences, and learning from others.
- Collaboration and coordination: Working closely with other healthcare professionals involved in the patient’s care, such as physicians, dietitians, and nurses.
- Ongoing evaluation and adjustment: Regularly assessing the patient’s progress and making adjustments to the program as needed.
4. How would you evaluate the effectiveness of a diabetes management program?
- Patient outcomes: Measuring improvements in HbA1c levels, blood pressure, lipid profile, and other health indicators.
- Patient satisfaction: Conducting surveys or interviews to assess patients’ satisfaction with the program and their perceived improvement in knowledge and skills.
- Program adherence: Tracking patient participation rates in education sessions, support groups, and other program activities.
- Cost-effectiveness: Evaluating the program’s cost in relation to the health benefits achieved for patients.
- Process measures: Assessing the quality and effectiveness of the educational materials, teaching methods, and overall program delivery.
5. How would you stay up-to-date on the latest advancements in diabetes management?
- Continuing education: Attending conferences, workshops, and webinars on diabetes management.
- Online resources: Reading medical journals, research articles, and guidelines from reputable organizations, such as the American Diabetes Association (ADA) and the American Association of Diabetes Educators (AADE).
- Networking: Connecting with other diabetes educators, healthcare professionals, and researchers through professional organizations and social media.
- Patient feedback: Incorporating patient input and experiences into program development and delivery.
6. How would you handle a patient who is resistant to making lifestyle changes?
- Establish a strong patient-provider relationship: Build rapport, listen attentively, and show empathy.
- Explore the patient’s motivations and barriers: Understand the patient’s reasons for resistance and identify potential areas of support.
- Provide personalized and practical solutions: Develop a plan that aligns with the patient’s lifestyle, preferences, and capabilities.
- Set realistic goals and celebrate progress: Help the patient set achievable goals and recognize their successes, however small.
- Collaborate with other healthcare professionals: Consult with a dietitian, psychologist, or other specialists as needed to provide additional support and guidance.
7. How would you manage a group of patients with diabetes in a community setting?
- Needs assessment: Identify the specific needs and interests of the patient population.
- Curriculum development: Create a tailored educational program that addresses the identified needs.
- Group facilitation: Lead group sessions that are interactive, engaging, and supportive.
- Evaluation and follow-up: Assess the effectiveness of the program and provide ongoing support to participants.
- Community partnerships: Collaborate with local organizations and healthcare providers to enhance program reach and impact.
8. How would you advocate for the needs of patients with diabetes?
- Policy engagement: Participate in public policy discussions and advocate for policies that support diabetes prevention and management.
- Community outreach: Educate the community about diabetes, reduce stigma, and promote early detection.
- Patient support: Provide resources, support, and advocacy for patients with diabetes and their families.
- Interdisciplinary collaboration: Work with other healthcare professionals to improve the quality and accessibility of diabetes care.
- Research and innovation: Stay informed about the latest research and advocate for advancements in diabetes management.
9. How would you ensure cultural sensitivity in your work as a Diabetes Education Coordinator?
- Cultural competence: Acquire knowledge about different cultures, beliefs, and practices related to diabetes management.
- Patient-centered care: Tailor education and support to meet the specific cultural needs and preferences of each patient.
- Respect and empathy: Value the beliefs and traditions of patients from diverse backgrounds and approach interactions with sensitivity and respect.
- Language access: Provide educational materials and services in multiple languages or use interpreters to ensure effective communication.
- Community partnerships: Collaborate with community organizations and leaders to understand and address the cultural barriers faced by patients.
10. What are your strengths and weaknesses as a Diabetes Education Coordinator?
Strengths:
- Strong knowledge of diabetes management and patient education principles
- Excellent communication and interpersonal skills
- Ability to create and deliver engaging and informative educational programs
- Passion for helping patients improve their health and well-being
- Commitment to patient-centered care and cultural sensitivity
Weaknesses:
- Limited experience in managing large patient groups in a community setting (but I am eager to develop this skill through training and mentorship)
- Not fluent in Spanish (but I am currently taking Spanish classes to improve my communication with Spanish-speaking patients)
Interviewers often ask about specific skills and experiences. With ResumeGemini‘s customizable templates, you can tailor your resume to showcase the skills most relevant to the position, making a powerful first impression. Also check out Resume Template specially tailored for Diabetes Education Coordinator.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Great Savings With New Year Deals and Discounts! In 2025, boost your job search and build your dream resume with ResumeGemini’s ATS optimized templates.
Researching the company and tailoring your answers is essential. Once you have a clear understanding of the Diabetes Education Coordinator‘s requirements, you can use ResumeGemini to adjust your resume to perfectly match the job description.
Key Job Responsibilities of a Diabetes Education Coordinator:
Diabetes Education Coordinators (DECs) play a crucial role in the healthcare team, specifically in managing and educating individuals with diabetes. Their key responsibilities include:
1. Patient Education and Support
DECs provide comprehensive diabetes education to patients, covering topics such as diet, medication management, blood glucose monitoring, and lifestyle modifications. They also provide emotional support, empower patients to manage their condition effectively, and address any doubts or concerns they may have.
2. Program Development and Implementation
DECs develop and implement patient education programs, workshops, and classes designed to meet the specific needs of individuals with diabetes. These programs focus on improving health outcomes, promoting self-care, and enhancing the quality of life for patients.
3. Collaboration and Coordination of Care
DECs collaborate closely with other healthcare professionals, including physicians, nurses, dietitians, and social workers, to ensure a comprehensive and coordinated approach to patient care. They participate in case conferences, share patient information, and provide ongoing support to the healthcare team.
4. Data Collection and Evaluation
DECs collect and analyze patient data, such as blood glucose levels, A1C levels, and medication adherence. They use this data to monitor patient progress, identify areas for improvement, and evaluate the effectiveness of education programs.
5. Advocacy and Outreach
DECs serve as advocates for individuals with diabetes, promoting awareness of the disease and its management. They conduct community outreach programs, participate in health fairs, and collaborate with community organizations to educate the public about diabetes prevention and management.
Interview Tips for Diabetes Education Coordinators:
To ace the interview for a Diabetes Education Coordinator position, candidates should consider the following tips:
1. Research the Organization and Position
Before the interview, thoroughly research the organization and the specific DEC position. This will demonstrate your interest and enthusiasm for the role. Understand the organization’s mission, goals, and values, and tailor your answers to align with their culture.
2. Highlight Relevant Skills and Experience
During the interview, emphasize your skills and experience in diabetes education, patient care, and program development. Provide specific examples of how you have effectively educated patients, collaborated with healthcare professionals, and implemented successful programs.
3. Showcase Your Passion for Diabetes Care
Convey your passion for helping individuals with diabetes manage their condition and improve their lives. Explain why you are interested in diabetes education and how your skills and experience make you an ideal candidate for the role.
4. Prepare Questions for the Interviewers
Asking thoughtful questions at the end of the interview demonstrates your engagement and interest in the position. Prepare questions related to the organization’s approach to diabetes care, opportunities for professional growth, and the specific responsibilities of the DEC role.
5. Practice Active Listening and Effective Communication
During the interview, practice active listening to ensure you clearly understand the questions being asked. Respond clearly and concisely, using examples to support your points. Effective communication skills are crucial for engaging patients and building rapport with healthcare professionals.
Next Step:
Now that you’re armed with a solid understanding of what it takes to succeed as a Diabetes Education Coordinator, it’s time to turn that knowledge into action. Take a moment to revisit your resume, ensuring it highlights your relevant skills and experiences. Tailor it to reflect the insights you’ve gained from this blog and make it shine with your unique qualifications. Don’t wait for opportunities to come to you—start applying for Diabetes Education Coordinator positions today and take the first step towards your next career milestone. Your dream job is within reach, and with a polished resume and targeted applications, you’ll be well on your way to achieving your career goals! Build your resume now with ResumeGemini.