Ever felt underprepared for that crucial job interview? Or perhaps you’ve landed the interview but struggled to articulate your skills and experiences effectively? Fear not! We’ve got you covered. In this blog post, we’re diving deep into the Medical Claims Processor interview questions that you’re most likely to encounter. But that’s not all. We’ll also provide expert insights into the key responsibilities of a Medical Claims Processor so you can tailor your answers to impress potential employers.
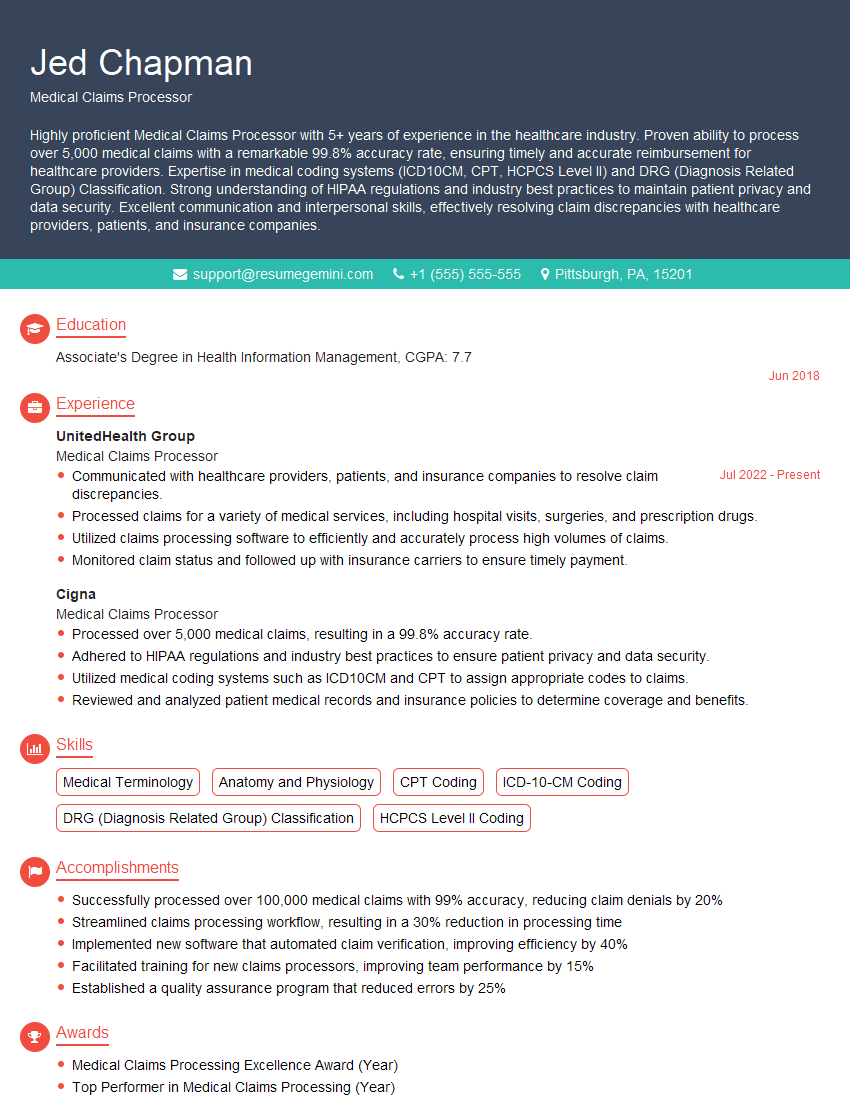
Acing the interview is crucial, but landing one requires a compelling resume that gets you noticed. Crafting a professional document that highlights your skills and experience is the first step toward interview success. ResumeGemini can help you build a standout resume that gets you called in for that dream job.
Essential Interview Questions For Medical Claims Processor
1. Describe the key steps involved in processing a medical claim.
The key steps involved in processing a medical claim typically include:
- Receiving and reviewing the claim
- Verifying patient eligibility and benefits
- Reviewing the claim for accuracy and completeness
- Processing the claim according to plan rules and regulations
- Denying or approving the claim and issuing payment or explanation of benefits (EOB)
2. What are the common reasons for claim denials?
Common reasons for claim denials may include:
Patient Eligibility and Coverage
- Patient is not covered by the plan
- Patient benefits have expired
- Services are not covered under the plan
Claim Errors
- Incomplete or inaccurate claim information
- Missing or invalid documentation
- Incorrect coding or billing errors
3. How do you handle complex claims with multiple procedures and diagnoses?
To handle complex claims with multiple procedures and diagnoses:
- Review the claim carefully to understand the patient’s medical history and treatment
- Research and apply the appropriate coding and billing guidelines
- Contact the provider’s office for clarification or additional information if needed
- Process the claim accurately and thoroughly to ensure proper reimbursement
4. What are your strategies for reducing claim processing time?
Strategies for reducing claim processing time include:
- Streamlining and automating claim processing tasks
- Maintaining open communication with providers and patients
- Educating providers on proper coding and documentation practices
- Using electronic health records (EHRs) and clearinghouse services
5. How do you ensure the accuracy of claim submissions?
To ensure the accuracy of claim submissions:
- Review all claims thoroughly before submission
- Verify patient information, diagnosis codes, and procedure codes
- Use claim scrubbing software to identify errors and inconsistencies
- Communicate with providers to resolve any discrepancies
6. Describe your experience with different types of health insurance plans.
I have experience with a variety of health insurance plans, including:
- Commercial health insurance
- Medicare
- Medicaid
- Workers’ compensation
- Tricare
7. What are the ethical considerations in medical claims processing?
Ethical considerations in medical claims processing include:
- Maintaining patient confidentiality
- Processing claims fairly and accurately
- Avoiding fraud and abuse
- Respecting patient autonomy
8. How do you stay updated on changes in healthcare regulations and coding guidelines?
I stay updated on changes in healthcare regulations and coding guidelines by:
- Attending industry conferences and webinars
- Reading trade publications and online resources
- Participating in continuing education programs
- Consulting with experts and colleagues
9. Tell me about a time when you had to resolve a complex billing issue.
In a previous role, I encountered a complex billing issue involving a patient with multiple insurance policies. The patient had received treatment at several different facilities, and each facility had billed for different services. I had to carefully review the patient’s medical records and insurance policies to determine which services were covered and which were not. I worked closely with the patient, the providers, and the insurance companies to resolve the issue and ensure that the patient received the appropriate benefits.
10. What is your understanding of the importance of data privacy and security in medical claims processing?
Data privacy and security are of utmost importance in medical claims processing due to the sensitive nature of the information handled. I am committed to protecting patient privacy by:
- Complying with all applicable privacy laws and regulations
- Using secure systems and technologies to store and transmit data
- Educating staff on the importance of data privacy and security
- Maintaining confidentiality at all times
Interviewers often ask about specific skills and experiences. With ResumeGemini‘s customizable templates, you can tailor your resume to showcase the skills most relevant to the position, making a powerful first impression. Also check out Resume Template specially tailored for Medical Claims Processor.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Great Savings With New Year Deals and Discounts! In 2025, boost your job search and build your dream resume with ResumeGemini’s ATS optimized templates.
Researching the company and tailoring your answers is essential. Once you have a clear understanding of the Medical Claims Processor‘s requirements, you can use ResumeGemini to adjust your resume to perfectly match the job description.
Key Job Responsibilities
Medical Claims Processors play a crucial role in the healthcare industry, ensuring accurate and timely claim processing. Their responsibilities encompass the following key areas:
1. Data Entry and Verification
Accurately entering patient information, medical procedures, and charges into the claims system.
- Verifying claim details against patient records and insurance policies
- Identifying and correcting errors or inconsistencies
2. Eligibility Verification
Ensuring that patients are eligible for coverage under the relevant insurance plan.
- Checking insurance coverage status
- Reviewing provider credentialing and contracts
3. Claim Adjudication
Reviewing claims for accuracy, completeness, and compliance with insurance policies.
- Applying medical coding and billing guidelines
- Determining the appropriate level of reimbursement
4. Claim Resolution
Resolving claim denials and appeals.
- Negotiating with insurance companies
- Providing documentation to support claims
5. Customer Service
Interacting with patients, providers, and insurance representatives.
- Answering inquiries about claim status
- Providing updates and explanations to resolve issues
Interview Tips
Preparing for a Medical Claims Processor interview requires a comprehensive approach, encompassing technical expertise, industry knowledge, and soft skills. Here are some valuable tips to help you ace the interview:
1. Research the Employer and Industry
Thoroughly research the healthcare organization you’re applying to, including its services, values, and industry reputation. This demonstrates your interest and commitment to the field.
- Review the company’s website, news articles, and LinkedIn page.
- Explore industry trends and key healthcare topics.
2. Practice Your Technical Skills
Ensure you have a solid understanding of medical coding and billing principles, as well as proficiency in claims processing software. Practice common tasks like data entry, eligibility verification, and claim adjudication.
- Review medical coding manuals and reference resources.
- Utilize online practice tools or simulations.
3. Highlight Your Customer Service Abilities
Medical Claims Processors often interact with patients and providers. Emphasize your communication skills, empathy, and ability to resolve issues effectively.
- Share examples of how you handled difficult customer situations.
- Describe your approach to building and maintaining positive relationships.
4. Showcase Your Attention to Detail
Accuracy and meticulousness are crucial in claims processing. Highlight your ability to focus on details, identify discrepancies, and ensure that claims are processed correctly.
- Emphasize your experience in reviewing and verifying data.
- Provide examples of how you have implemented quality control measures.
5. Prepare Industry-Specific Questions
Ask thoughtful questions about the organization’s claims processing workflow, industry trends, or any recent regulatory updates. This shows your engagement and interest in the profession.
- Inquire about specific process improvements or challenges.
- Ask about continuing education opportunities or professional development programs.
Next Step:
Now that you’re armed with interview-winning answers and a deeper understanding of the Medical Claims Processor role, it’s time to take action! Does your resume accurately reflect your skills and experience for this position? If not, head over to ResumeGemini. Here, you’ll find all the tools and tips to craft a resume that gets noticed. Don’t let a weak resume hold you back from landing your dream job. Polish your resume, hit the “Build Your Resume” button, and watch your career take off! Remember, preparation is key, and ResumeGemini is your partner in interview success.