Are you gearing up for a career in Medical Claims Specialist? Feeling nervous about the interview questions that might come your way? Don’t worry, you’re in the right place. In this blog post, we’ll dive deep into the most common interview questions for Medical Claims Specialist and provide you with expert-backed answers. We’ll also explore the key responsibilities of this role so you can tailor your responses to showcase your perfect fit.
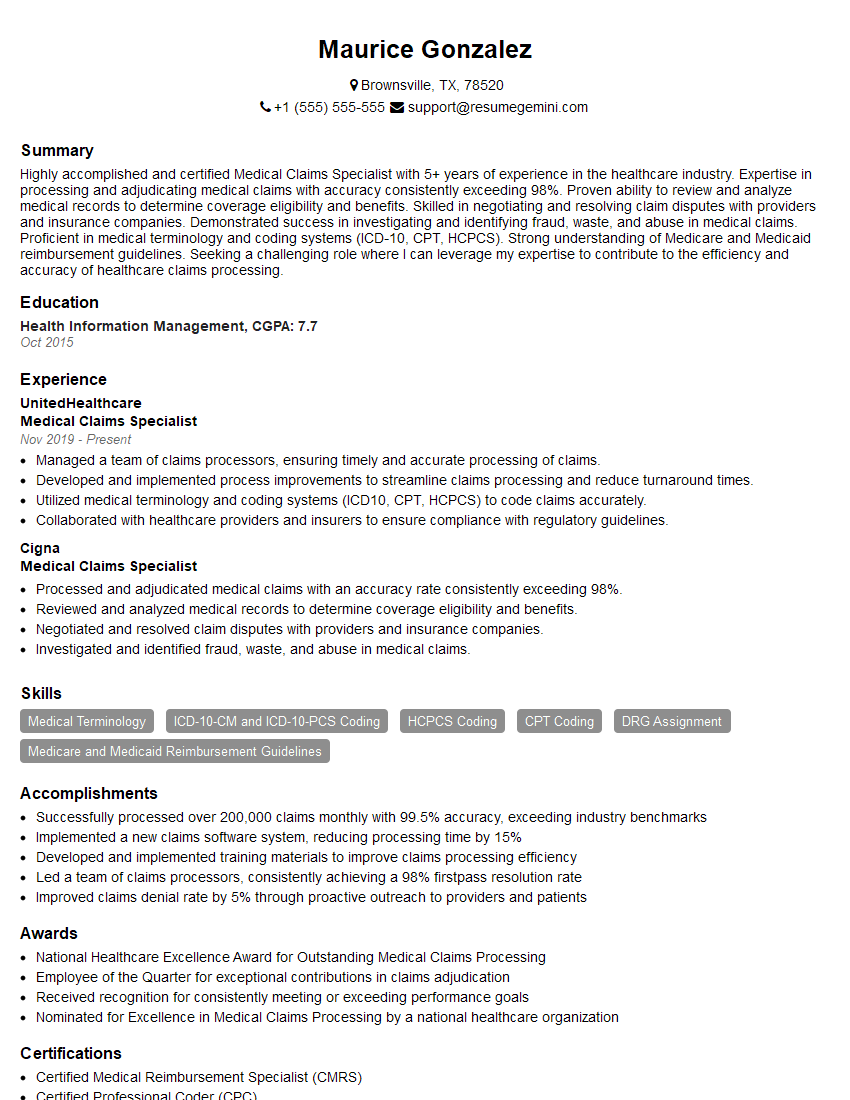
Acing the interview is crucial, but landing one requires a compelling resume that gets you noticed. Crafting a professional document that highlights your skills and experience is the first step toward interview success. ResumeGemini can help you build a standout resume that gets you called in for that dream job.
Essential Interview Questions For Medical Claims Specialist
1. Describe the key steps involved in processing a medical claim?
- Receive and review the medical claim.
- Enter the claim data into the claims system.
- Validate the claim against pre-determined rules and system edits.
- Determine the patient’s eligibility for coverage.
- Verify the date of service and place of service.
- Analyze the claim for completeness, accuracy, and necessity.
- Identify and apply appropriate coding.
- Assign the claim to the appropriate provider or facility.
- Process the claim and issue payment or denial.
- Monitor the claim throughout the adjudication process.
2. Explain the different types of medical claim denials and how to appeal them?
Reasons for Denials
- Insufficient documentation
- Invalid coding
- Lack of medical necessity
- Ineligibility for coverage
- Duplicate billing
Appeals Process
- Review the denial notice to understand the reason.
- Gather additional documentation or evidence to support the claim.
- Submit an appeal letter to the insurance company.
- Provide a clear and concise explanation of why the claim should be reconsidered.
- Follow up with the insurance company to track the status of the appeal.
3. How do you handle complex medical claims that require research and investigation?
- Gather all relevant information and documentation.
- Review the patient’s medical records and treatment plan.
- Consult with medical professionals and experts as needed.
- Research industry guidelines and regulations.
- Analyze the claim thoroughly to identify any discrepancies or inconsistencies.
- Communicate with the patient and provider to obtain additional information.
- Document the research and investigation process, including the sources consulted.
- Make a determination based on the evidence gathered.
4. Discuss the importance of maintaining confidentiality and HIPAA compliance in medical claims processing?
- Protecting patient privacy and sensitive health information.
- Complying with legal and ethical obligations.
- Avoiding financial penalties and reputational damage.
- Ensuring patient trust and confidence.
- Implementing physical, technical, and administrative safeguards to protect data.
- Training staff on HIPAA regulations and best practices.
- Reporting and investigating any suspected breaches.
5. How do you stay up-to-date with changes in medical coding, regulations, and industry best practices?
- Attending conferences and workshops.
- Reading industry publications and journals.
- Consulting with medical professionals and experts.
- Participating in online forums and discussion groups.
- Reviewing government websites and updates.
- Obtaining certifications and continuing education credits.
6. Tell me about a time when you had to resolve a billing dispute with a provider or patient?
- Identified the issue and gathered all relevant information.
- Communicated with the provider or patient to understand their perspective.
- Reviewed the claim and applicable regulations.
- Explained the reason for the billing decision.
- Negotiated a resolution that was fair and compliant.
- Documented the resolution and followed up to ensure satisfaction.
7. Describe your experience with medical billing software and how you use it to efficiently process claims?
- Proficiency in using specific software applications (e.g., Epic, Cerner).
- Utilizing automation tools to streamline data entry and reduce errors.
- Customizing the software to meet the needs of the organization.
- Generating reports for analysis and decision-making.
- Maintaining and updating the software to ensure optimal functionality.
8. How do you handle high claim volumes and meet deadlines while maintaining quality standards?
- Prioritizing claims based on urgency and complexity.
- Delegating tasks to ensure efficient workflow.
- Automating repetitive processes to save time.
- Training and empowering team members to make decisions.
- Implementing quality control measures to minimize errors.
- Communicating with stakeholders to manage expectations.
9. Describe your knowledge of medical terminology and anatomy. How do you use this knowledge in your work?
- Understanding medical terms and abbreviations.
- Interpreting medical records and reports.
- Accurately coding medical procedures and diagnoses.
- Communicating effectively with healthcare professionals.
- Staying up-to-date with advancements in medical science.
10. What continuous improvement initiatives have you implemented or participated in to enhance the medical claims process?
- Automating claim submission and adjudication.
- Developing and implementing best practices for claim processing.
- Participating in process improvement workshops and training.
- Suggesting and testing new technologies to improve efficiency.
- Analyzing data to identify and address bottlenecks.
Interviewers often ask about specific skills and experiences. With ResumeGemini‘s customizable templates, you can tailor your resume to showcase the skills most relevant to the position, making a powerful first impression. Also check out Resume Template specially tailored for Medical Claims Specialist.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Great Savings With New Year Deals and Discounts! In 2025, boost your job search and build your dream resume with ResumeGemini’s ATS optimized templates.
Researching the company and tailoring your answers is essential. Once you have a clear understanding of the Medical Claims Specialist‘s requirements, you can use ResumeGemini to adjust your resume to perfectly match the job description.
Key Job Responsibilities
Medical Claims Specialists are responsible for the accurate and timely processing of medical claims. This includes verifying patient information, reviewing medical records, and determining eligibility for coverage. They also may be responsible for negotiating with insurance companies and resolving billing disputes.
1. Process medical claims
The primary responsibility of a Medical Claims Specialist is to process medical claims. This includes reviewing claims for completeness, accuracy, and eligibility, and then submitting them to the appropriate insurance company. They also may be responsible for following up on claims to ensure that they are processed correctly and paid promptly.
- Review claims for completeness, accuracy, and eligibility
- Submit claims to the appropriate insurance company
- Follow up on claims to ensure that they are processed correctly and paid promptly
2. Verify patient information
Medical Claims Specialists must verify patient information to ensure that claims are processed correctly. This includes verifying the patient’s name, address, date of birth, and insurance information. They may also be responsible for verifying the patient’s medical history and treatment plan.
- Verify the patient’s name, address, date of birth, and insurance information
- Verify the patient’s medical history and treatment plan
3. Review medical records
Medical Claims Specialists must review medical records to determine the medical necessity of treatment and to ensure that the services billed are covered under the patient’s insurance plan. They may also be responsible for interpreting medical terminology and coding.
- Determine the medical necessity of treatment
- Ensure that the services billed are covered under the patient’s insurance plan
- Interpret medical terminology and coding
4. Determine eligibility for coverage
Medical Claims Specialists must determine eligibility for coverage to ensure that the patient is covered under the insurance plan for the services billed. This may involve verifying the patient’s enrollment, deductible, and copayment. They may also be responsible for determining coordination of benefits between multiple insurance plans.
- Verify the patient’s enrollment, deductible, and copayment
- Determine coordination of benefits between multiple insurance plans
Interview Tips
An interview for a Medical Claims Specialist position can be challenging, but there are a few things you can do to prepare and increase your chances of success.
1. Research the company and the position
Before you go to your interview, take some time to research the company and the position. This will help you to understand the company’s culture, values, and goals, and to tailor your answers to the interviewer’s questions.
- Visit the company’s website
- Read articles about the company in the news
- Talk to people who work at the company
2. Practice answering common interview questions
There are a few common interview questions that you can expect to be asked, such as “Tell me about yourself” and “Why are you interested in this position?” It is helpful to practice answering these questions in advance so that you can deliver your answers confidently and concisely.
- Practice answering common interview questions
- Use the STAR method to answer questions
- Be confident in your answers
3. Be prepared to talk about your experience
The interviewer will likely ask you to talk about your experience in medical claims processing. Be prepared to discuss your skills and experience in detail, and to provide examples of your work.
- Highlight your experience in medical claims processing
- Be prepared to discuss your skills and experience in detail
- Provide examples of your work
4. Be professional and courteous
First impressions matter, so it is important to be professional and courteous throughout the interview. Dress appropriately, arrive on time, and be respectful of the interviewer’s time.
- Dress appropriately
- Arrive on time
- Be respectful of the interviewer’s time
Next Step:
Now that you’re armed with interview-winning answers and a deeper understanding of the Medical Claims Specialist role, it’s time to take action! Does your resume accurately reflect your skills and experience for this position? If not, head over to ResumeGemini. Here, you’ll find all the tools and tips to craft a resume that gets noticed. Don’t let a weak resume hold you back from landing your dream job. Polish your resume, hit the “Build Your Resume” button, and watch your career take off! Remember, preparation is key, and ResumeGemini is your partner in interview success.