Are you a seasoned Medical Claims Analyst seeking a new career path? Discover our professionally built Medical Claims Analyst Resume Template. This time-saving tool provides a solid foundation for your job search. Simply click “Edit Resume” to customize it with your unique experiences and achievements. Customize fonts and colors to match your personal style and increase your chances of landing your dream job. Explore more Resume Templates for additional options.
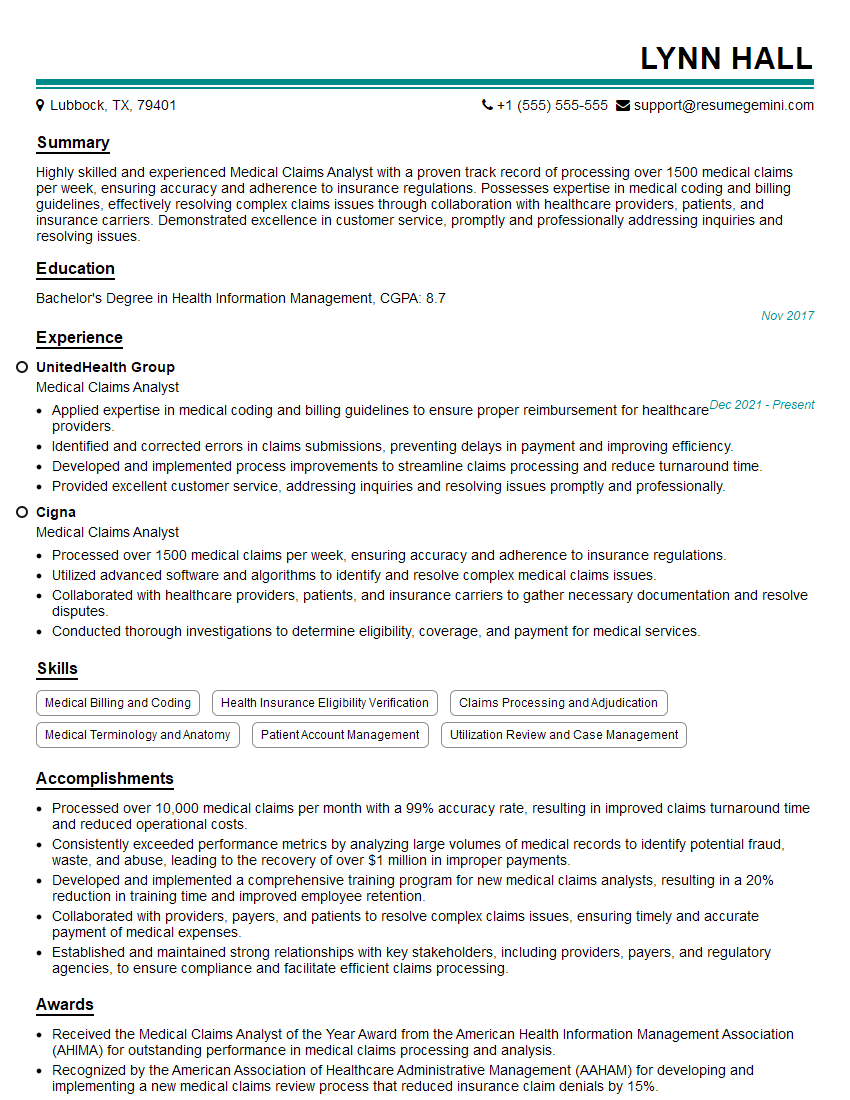
Lynn Hall
Medical Claims Analyst
Summary
Highly skilled and experienced Medical Claims Analyst with a proven track record of processing over 1500 medical claims per week, ensuring accuracy and adherence to insurance regulations. Possesses expertise in medical coding and billing guidelines, effectively resolving complex claims issues through collaboration with healthcare providers, patients, and insurance carriers. Demonstrated excellence in customer service, promptly and professionally addressing inquiries and resolving issues.
Education
Bachelor’s Degree in Health Information Management
November 2017
Skills
- Medical Billing and Coding
- Health Insurance Eligibility Verification
- Claims Processing and Adjudication
- Medical Terminology and Anatomy
- Patient Account Management
- Utilization Review and Case Management
Work Experience
Medical Claims Analyst
- Applied expertise in medical coding and billing guidelines to ensure proper reimbursement for healthcare providers.
- Identified and corrected errors in claims submissions, preventing delays in payment and improving efficiency.
- Developed and implemented process improvements to streamline claims processing and reduce turnaround time.
- Provided excellent customer service, addressing inquiries and resolving issues promptly and professionally.
Medical Claims Analyst
- Processed over 1500 medical claims per week, ensuring accuracy and adherence to insurance regulations.
- Utilized advanced software and algorithms to identify and resolve complex medical claims issues.
- Collaborated with healthcare providers, patients, and insurance carriers to gather necessary documentation and resolve disputes.
- Conducted thorough investigations to determine eligibility, coverage, and payment for medical services.
Accomplishments
- Processed over 10,000 medical claims per month with a 99% accuracy rate, resulting in improved claims turnaround time and reduced operational costs.
- Consistently exceeded performance metrics by analyzing large volumes of medical records to identify potential fraud, waste, and abuse, leading to the recovery of over $1 million in improper payments.
- Developed and implemented a comprehensive training program for new medical claims analysts, resulting in a 20% reduction in training time and improved employee retention.
- Collaborated with providers, payers, and patients to resolve complex claims issues, ensuring timely and accurate payment of medical expenses.
- Established and maintained strong relationships with key stakeholders, including providers, payers, and regulatory agencies, to ensure compliance and facilitate efficient claims processing.
Awards
- Received the Medical Claims Analyst of the Year Award from the American Health Information Management Association (AHIMA) for outstanding performance in medical claims processing and analysis.
- Recognized by the American Association of Healthcare Administrative Management (AAHAM) for developing and implementing a new medical claims review process that reduced insurance claim denials by 15%.
- Awarded the Excellence in Medical Claims Processing Award from the Healthcare Information and Management Systems Society (HIMSS) for exceptional contributions to the field.
- Received the Medical Claims Analyst Certification (CMCA) from AHIMA, demonstrating a deep understanding of medical coding, billing, and claims processing regulations.
Certificates
- Certified Professional Coder (CPC)
- Certified Medical Insurance Specialist (CMIS)
- Certified Health Insurance Auditor (CHIA)
- Certified Medical Compliance Auditor (CMCA)
Career Expert Tips:
- Select the ideal resume template to showcase your professional experience effectively.
- Master the art of resume writing to highlight your unique qualifications and achievements.
- Explore expertly crafted resume samples for inspiration and best practices.
- Build your best resume for free this new year with ResumeGemini. Enjoy exclusive discounts on ATS optimized resume templates.
How To Write Resume For Medical Claims Analyst
- Highlight your skills in medical billing and coding, health insurance eligibility verification, and claims processing and adjudication.
- Showcase your knowledge of medical terminology and anatomy, patient account management, and utilization review and case management.
- Emphasize your ability to provide excellent customer service and resolve issues promptly and professionally.
- Quantify your accomplishments whenever possible, using specific metrics to demonstrate your impact on the organization.
Essential Experience Highlights for a Strong Medical Claims Analyst Resume
- Process medical claims accurately and efficiently, ensuring compliance with insurance regulations.
- Utilize advanced software and algorithms to identify and resolve complex medical claims issues.
- Collaborate with healthcare providers, patients, and insurance carriers to gather necessary documentation and resolve disputes.
- Conduct thorough investigations to determine eligibility, coverage, and payment for medical services.
- Apply expertise in medical coding and billing guidelines to ensure proper reimbursement for healthcare providers.
- Identify and correct errors in claims submissions, preventing delays in payment and improving efficiency.
- Develop and implement process improvements to streamline claims processing and reduce turnaround time.
Frequently Asked Questions (FAQ’s) For Medical Claims Analyst
What are the key skills required to be a successful Medical Claims Analyst?
Medical Claims Analysts need to have a strong understanding of medical billing and coding, health insurance eligibility verification, claims processing and adjudication, medical terminology and anatomy, patient account management, utilization review and case management, and customer service.
What are the career prospects for Medical Claims Analysts?
Medical Claims Analysts can advance to roles such as Claims Supervisor, Claims Manager, or Director of Claims. They may also specialize in areas such as fraud investigation or utilization review.
What is the average salary for Medical Claims Analysts?
According to the U.S. Bureau of Labor Statistics, the median annual salary for Medical Records and Health Information Technicians (which includes Medical Claims Analysts) was $46,300 as of May 2021.
What are the typical work hours for Medical Claims Analysts?
Medical Claims Analysts typically work full-time hours, which may include evenings or weekends to meet deadlines.
What kind of work environment can I expect as a Medical Claims Analyst?
Medical Claims Analysts typically work in an office environment, where they may interact with other claims analysts, healthcare providers, patients, and insurance carriers.
What are the challenges that Medical Claims Analysts face?
Medical Claims Analysts may face challenges such as dealing with complex medical claims, meeting deadlines, and resolving disputes with healthcare providers or insurance carriers.
What is the job outlook for Medical Claims Analysts?
The job outlook for Medical Records and Health Information Technicians (which includes Medical Claims Analysts) is expected to grow 9% from 2021 to 2031, faster than the average for all occupations.
What are the steps to becoming a Medical Claims Analyst?
To become a Medical Claims Analyst, you will typically need to have a high school diploma or equivalent, and complete a formal training program or earn a degree in a related field such as health information management or medical billing and coding.