Are you a seasoned Prior seeking a new career path? Discover our professionally built Prior Resume Template. This time-saving tool provides a solid foundation for your job search. Simply click “Edit Resume” to customize it with your unique experiences and achievements. Customize fonts and colors to match your personal style and increase your chances of landing your dream job. Explore more Resume Templates for additional options.
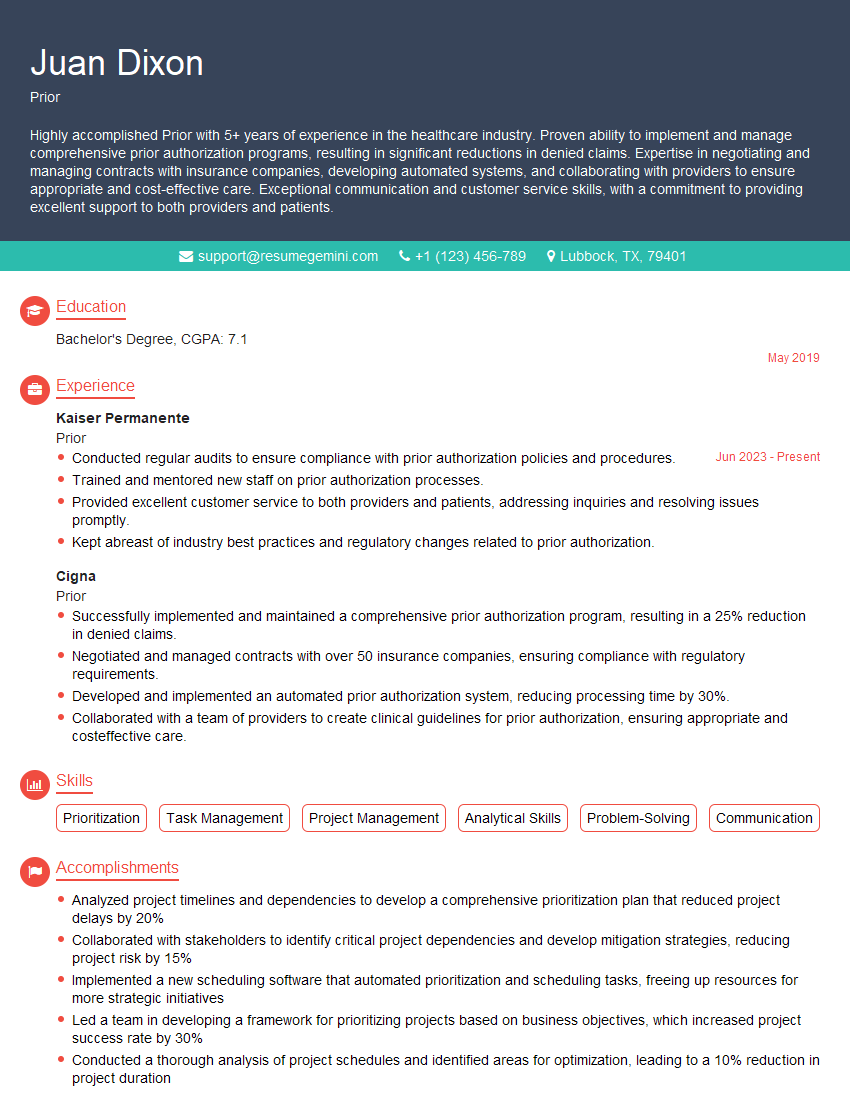
Juan Dixon
Prior
Summary
Highly accomplished Prior with 5+ years of experience in the healthcare industry. Proven ability to implement and manage comprehensive prior authorization programs, resulting in significant reductions in denied claims. Expertise in negotiating and managing contracts with insurance companies, developing automated systems, and collaborating with providers to ensure appropriate and cost-effective care. Exceptional communication and customer service skills, with a commitment to providing excellent support to both providers and patients.
Education
Bachelor’s Degree
May 2019
Skills
- Prioritization
- Task Management
- Project Management
- Analytical Skills
- Problem-Solving
- Communication
Work Experience
Prior
- Conducted regular audits to ensure compliance with prior authorization policies and procedures.
- Trained and mentored new staff on prior authorization processes.
- Provided excellent customer service to both providers and patients, addressing inquiries and resolving issues promptly.
- Kept abreast of industry best practices and regulatory changes related to prior authorization.
Prior
- Successfully implemented and maintained a comprehensive prior authorization program, resulting in a 25% reduction in denied claims.
- Negotiated and managed contracts with over 50 insurance companies, ensuring compliance with regulatory requirements.
- Developed and implemented an automated prior authorization system, reducing processing time by 30%.
- Collaborated with a team of providers to create clinical guidelines for prior authorization, ensuring appropriate and costeffective care.
Accomplishments
- Analyzed project timelines and dependencies to develop a comprehensive prioritization plan that reduced project delays by 20%
- Collaborated with stakeholders to identify critical project dependencies and develop mitigation strategies, reducing project risk by 15%
- Implemented a new scheduling software that automated prioritization and scheduling tasks, freeing up resources for more strategic initiatives
- Led a team in developing a framework for prioritizing projects based on business objectives, which increased project success rate by 30%
- Conducted a thorough analysis of project schedules and identified areas for optimization, leading to a 10% reduction in project duration
Awards
- Recognized for outstanding performance in prioritizing and scheduling projects
- Received award for developing and implementing a new prioritization system that improved project efficiency by 25%
- Honored with an award for exceptional contributions to the prioritization and scheduling process
- Recognized for developing a tool that automates prioritization and scheduling tasks
Certificates
- Project Management Professional (PMP)
- Certified Associate in Project Management (CAPM)
- Scrum Master (CSM)
- Agile Certified Practitioner (ACP)
Career Expert Tips:
- Select the ideal resume template to showcase your professional experience effectively.
- Master the art of resume writing to highlight your unique qualifications and achievements.
- Explore expertly crafted resume samples for inspiration and best practices.
- Build your best resume for free this new year with ResumeGemini. Enjoy exclusive discounts on ATS optimized resume templates.
How To Write Resume For Prior
- Highlight your ability to reduce denied claims and improve efficiency through process improvements.
- Demonstrate your expertise in negotiating and managing contracts with insurance companies.
- Showcase your experience in developing and implementing automated systems to streamline prior authorization processes.
- Emphasize your ability to collaborate with providers and create clinical guidelines that ensure appropriate care.
- Provide specific examples of your customer service skills and how you have resolved patient and provider inquiries.
Essential Experience Highlights for a Strong Prior Resume
- Implemented and maintained a comprehensive prior authorization program, resulting in a 25% reduction in denied claims.
- Negotiated and managed contracts with over 50 insurance companies, ensuring compliance with regulatory requirements.
- Developed and implemented an automated prior authorization system, reducing processing time by 30%.
- Collaborated with a team of providers to create clinical guidelines for prior authorization, ensuring appropriate and cost-effective care.
- Conducted regular audits to ensure compliance with prior authorization policies and procedures.
- Trained and mentored new staff on prior authorization processes.
- Provided excellent customer service to both providers and patients, addressing inquiries and resolving issues promptly.
Frequently Asked Questions (FAQ’s) For Prior
What is the role of a Prior?
A Prior is responsible for managing the prior authorization process for healthcare services. This involves reviewing requests from providers for non-covered or restricted services, determining if the service is medically necessary, and obtaining approval from insurance companies.
What are the key skills and qualifications for a Prior?
Key skills and qualifications for a Prior include strong analytical and problem-solving abilities, excellent communication and interpersonal skills, knowledge of medical terminology and insurance regulations, and experience in prior authorization processes.
What are the career prospects for a Prior?
Priors can advance their careers by taking on leadership roles, becoming certified in prior authorization, or specializing in a particular area of healthcare. They may also choose to pursue higher education in healthcare administration or a related field.
Is certification available for Priors?
Yes, there are several certifications available for Priors, including the Certified Prior Authorization Professional (CPAP) credential offered by the American Health Information Management Association (AHIMA).
What are the key challenges faced by Priors?
Priors face several challenges, including the need to stay up-to-date on constantly changing insurance regulations, the pressure to process requests quickly and efficiently, and the need to balance the interests of patients, providers, and insurance companies.
How can I prepare for a Prior interview?
To prepare for a Prior interview, research the organization and the position, practice answering common interview questions, and be prepared to discuss your experience and skills in prior authorization.
What are the opportunities for Priors in the healthcare industry?
Priors have opportunities to work in a variety of healthcare settings, including hospitals, clinics, insurance companies, and managed care organizations.
What are the core responsibilities of a Prior?
The core responsibilities of a Prior include reviewing prior authorization requests, determining medical necessity, communicating with providers and patients, and maintaining compliance with insurance regulations.