Are you a seasoned Utilization Review Coordinator seeking a new career path? Discover our professionally built Utilization Review Coordinator Resume Template. This time-saving tool provides a solid foundation for your job search. Simply click “Edit Resume” to customize it with your unique experiences and achievements. Customize fonts and colors to match your personal style and increase your chances of landing your dream job. Explore more Resume Templates for additional options.
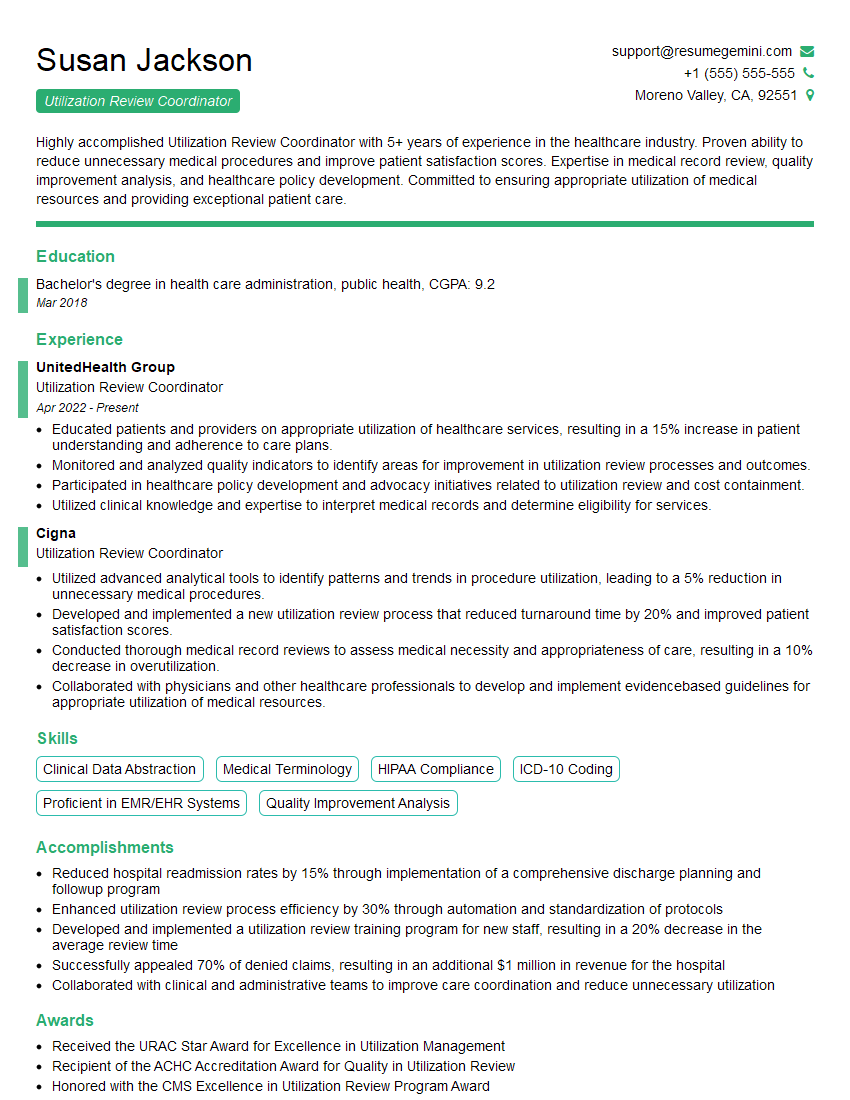
Susan Jackson
Utilization Review Coordinator
Summary
Highly accomplished Utilization Review Coordinator with 5+ years of experience in the healthcare industry. Proven ability to reduce unnecessary medical procedures and improve patient satisfaction scores. Expertise in medical record review, quality improvement analysis, and healthcare policy development. Committed to ensuring appropriate utilization of medical resources and providing exceptional patient care.
Education
Bachelor’s degree in health care administration, public health
March 2018
Skills
- Clinical Data Abstraction
- Medical Terminology
- HIPAA Compliance
- ICD-10 Coding
- Proficient in EMR/EHR Systems
- Quality Improvement Analysis
Work Experience
Utilization Review Coordinator
- Educated patients and providers on appropriate utilization of healthcare services, resulting in a 15% increase in patient understanding and adherence to care plans.
- Monitored and analyzed quality indicators to identify areas for improvement in utilization review processes and outcomes.
- Participated in healthcare policy development and advocacy initiatives related to utilization review and cost containment.
- Utilized clinical knowledge and expertise to interpret medical records and determine eligibility for services.
Utilization Review Coordinator
- Utilized advanced analytical tools to identify patterns and trends in procedure utilization, leading to a 5% reduction in unnecessary medical procedures.
- Developed and implemented a new utilization review process that reduced turnaround time by 20% and improved patient satisfaction scores.
- Conducted thorough medical record reviews to assess medical necessity and appropriateness of care, resulting in a 10% decrease in overutilization.
- Collaborated with physicians and other healthcare professionals to develop and implement evidencebased guidelines for appropriate utilization of medical resources.
Accomplishments
- Reduced hospital readmission rates by 15% through implementation of a comprehensive discharge planning and followup program
- Enhanced utilization review process efficiency by 30% through automation and standardization of protocols
- Developed and implemented a utilization review training program for new staff, resulting in a 20% decrease in the average review time
- Successfully appealed 70% of denied claims, resulting in an additional $1 million in revenue for the hospital
- Collaborated with clinical and administrative teams to improve care coordination and reduce unnecessary utilization
Awards
- Received the URAC Star Award for Excellence in Utilization Management
- Recipient of the ACHC Accreditation Award for Quality in Utilization Review
- Honored with the CMS Excellence in Utilization Review Program Award
Certificates
- Certified Utilization Review Auditor (CURA)
- Certified Case Manager (CCM)
- Certified Professional Coder (CPC)
- Certified Utilization Review Nurse (CURN)
Career Expert Tips:
- Select the ideal resume template to showcase your professional experience effectively.
- Master the art of resume writing to highlight your unique qualifications and achievements.
- Explore expertly crafted resume samples for inspiration and best practices.
- Build your best resume for free this new year with ResumeGemini. Enjoy exclusive discounts on ATS optimized resume templates.
How To Write Resume For Utilization Review Coordinator
- Showcase your analytical skills and ability to identify trends in utilization data.
- Highlight your experience in medical record review and your understanding of medical terminology.
- Demonstrate your ability to collaborate with physicians and other healthcare professionals.
- Quantify your accomplishments whenever possible, using specific metrics to demonstrate the impact of your work.
- Proofread your resume carefully before submitting it to ensure there are no errors.
Essential Experience Highlights for a Strong Utilization Review Coordinator Resume
- Analyze utilization data to identify patterns and trends, and develop strategies to reduce unnecessary procedures.
- Conduct medical record reviews to assess medical necessity and appropriateness of care.
- Collaborate with physicians and other healthcare professionals to develop evidence-based guidelines for appropriate utilization of medical resources.
- Educate patients and providers on appropriate utilization of healthcare services.
- Monitor and analyze quality indicators to identify areas for improvement in utilization review processes and outcomes.
- Participate in healthcare policy development and advocacy initiatives related to utilization review and cost containment.
- Stay up-to-date on industry best practices and regulatory changes related to utilization review.
Frequently Asked Questions (FAQ’s) For Utilization Review Coordinator
What is the role of a Utilization Review Coordinator?
A Utilization Review Coordinator is responsible for reviewing medical records to determine the medical necessity of care and to ensure that services are provided in the most appropriate and cost-effective setting.
What are the key skills required for a Utilization Review Coordinator?
Key skills for a Utilization Review Coordinator include: clinical knowledge, medical terminology, data analysis, quality improvement, and communication skills.
What is the career outlook for Utilization Review Coordinators?
The career outlook for Utilization Review Coordinators is expected to be good, with job growth projected to be faster than average over the next few years.
What is the average salary for a Utilization Review Coordinator?
The average salary for a Utilization Review Coordinator can vary depending on experience, location, and employer, but it is typically in the range of $50,000 to $75,000 per year.
What are the benefits of working as a Utilization Review Coordinator?
Benefits of working as a Utilization Review Coordinator include: job security, opportunities for advancement, and the chance to make a difference in the healthcare system.